A Deep Learning Pipeline for Automated Classification of Pathology in Laryngoscopy Videos
This interdisciplinary collaboration between laryngologists and computer scientists aims to use deep learning to automate both dataset creation and disease classification in video-laryngoscopy. Using deep learning to classify pathology on laryngoscopy images involves two steps: (1) building a labeled dataset and (2) using the dataset to train a classifier to distinguish healthy from pathologic images. A deep learning model requires a large amount of training data, and building a dataset by manually extracting informative frames from laryngoscopy videos is a research bottleneck. We have developed a deep learning classifier capable of automatically identifying key frames from laryngoscopic videos.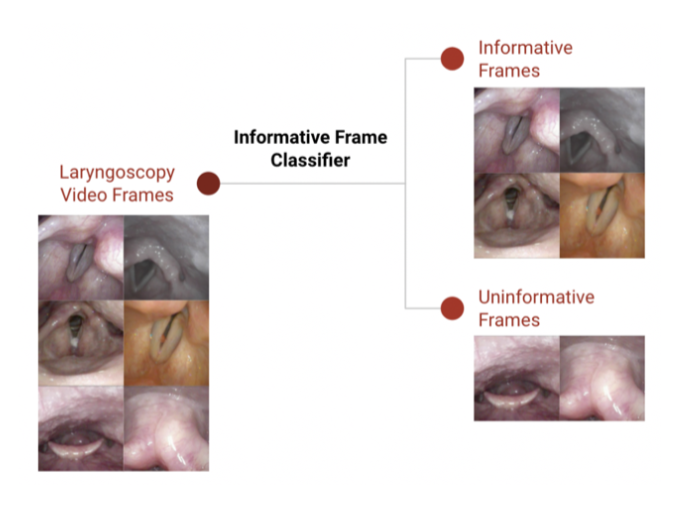
Achievements:
Our deep learning classifier of key frames has 87% precision, demonstrating the potential to facilitate accurate and efficient creation of deep learning datasets across a range of laryngeal diseases. As a pilot study, we used the informative frame classifier to create a dataset to train a model to recognize vocal fold polyps, which achieved a classification accuracy of 77.4%.
The continuation of this work was awarded the 2021 American Laryngological Voice and Research Education Grant.
Vacuum Helmet to Contain Pathogen-Bearing Droplets in Dental, Otolaryngological and Ophthlamologic Outpatient Interventions.
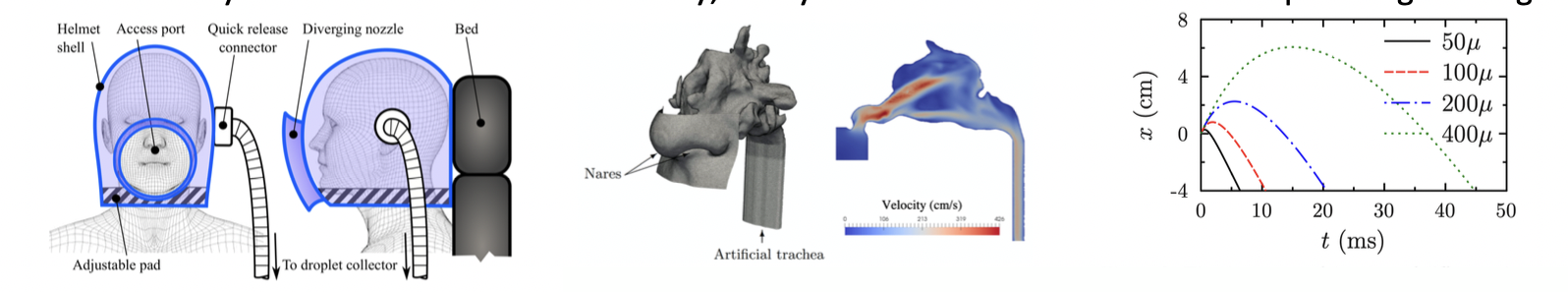
Figure 1: The vacuum helmet proposed design. Figure 2. Airflow simulation in the upper airways using computational fluid dynamics. Figure 3. The departure of droplets of different sizes from the mouth during the most extreme expiratory events when the vacuum helmet is used. Difference between intervention and reference counts for positive controls stratified by particle size. Positive values represent higher intervention counts relative to background; negative values represent lower intervention counts.
Is Office Laryngoscopy an Aerosol-Generating Procedure?
The novel coronavirus, SARS-CoV-2, has highlighted a multitude of deficiencies in our healthcare system and scientific knowledge. One of the most disconcerting of these has been our incomplete understanding of aerosol-generating procedures (AGPs). Procedures and interventions involving the upper and lower airways have been linked to increased infection rates among healthcare professionals. Although a number of studies have investigated the aerosol-generating potential of specific procedures, evidence has been ambiguous or contradictory. Office laryngoscopy is a prime example, being a source of concern, debate, and speculation during this crisis. In this study, we quantify aerosolization associated with flexible and rigid office laryngoscopy, and critically review methods for measuring the aerosolizing potential of medical and surgical interventions.

Achievements:
Rameau A, Lee M, Enver N, Sulica L. Is Office Laryngoscopy an Aerosol Generating Procedure? Accepted for publication: July 1st, 2020. Laryngoscope (expedited, no revision needed acceptance)
Our study suggests that office laryngoscopy may not be an AGP according to the standard medical definition, namely aerosol production more than normally expected from breathing, coughing, sneezing, and speaking.
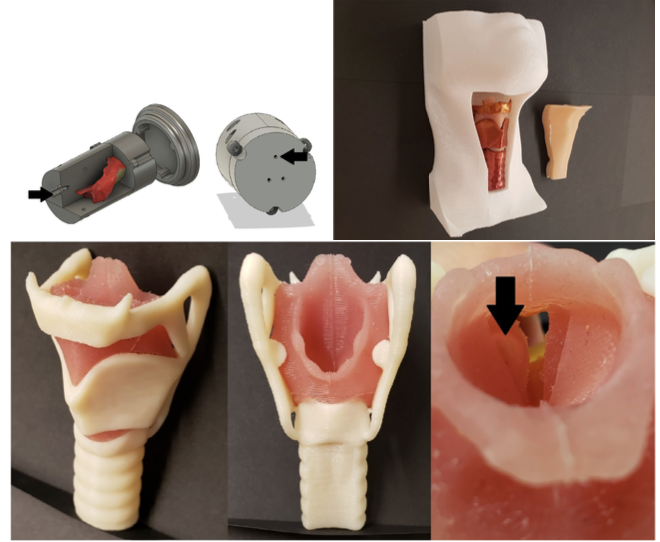
An Open-Source 3D Printed Laryngeal Model for Injection Laryngoplasty Training
MyophonX
Achievements:
• Rameau A. Pilot study for a novel and personalized voice restoration device for patients with laryngectomy. Head Neck. 2020;42(5):839-845.
• New International Application No. PCT/US2020/034917, Based on U.S. Provisional App. No. 62/854,128, submitted June 2020
• Winner, 2018 Annual Weill Cornell Medicine Health Innovation Hackathon
• This work was supported by a grant (UL1-TR-002384) from the Clinical and Translational Science Center at Weill Cornell Medicine, which is funded by the National Center for Advancing Translational Sciences (NCATS)
• Project selected for start-up acceleration by ElabNYC, a competitive 6-month program launched by the City of New York, designed for NY scientists interested in forming new ventures in the life sciences and healthcare technology sectors.
• One of the four Cornell start-ups selected for podium presentation at the Cornell Entrepreneurship Summit in November 2019 at the Times Building, New York, NY.

